Dr Quince says single-cell sequencing of raw samples offers possibilities for assessing spread through a mixed population of microbes. This approach could also be used on uncultured cells, which would limit the need for lab growth of cells before analysis.
“Some microbes may not be easy to culture in a lab,” he explains, “and being able to sequence them without culturing would make a difference.”
He also believes a mixed culture gives a clearer idea of which species to concentrate on when sequencing.
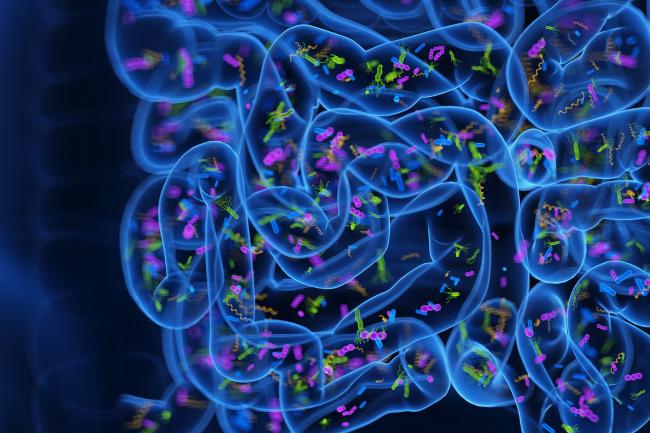
“We need a much broader view of these communities. The gut is a very complex environment.
“We can test two gut species to see if they transmit AMR to each other, but we are putting them in an agar plate together. In the real world they may live in very different parts of the gut and never come in contact.
“It’s not just about the possibility it could happen, it’s about assessing the real likelihood of transmission between two species.”
He explains antibiotic use does not just pressure pathogenic bacteria to evolve. It also puts pressure on harmless “friendly” microorganisms to develop AMR.
This response means our gut microbiomes may act as a reservoir for AMR genes to pass between pathogens. Therefore it is vital to look at interactions between species – including species that are not of concern in themselves.
Further research at the Earlham Institute is being conducted by Dr Rob James, who is conducting experiments to track the movement of AMR between pathogens and the beneficial microbes that are resident in the gut microbiome. He is working in collaboration with Dr Falk Hildebrand and Dr Naiara Bereza at the Quadram Institute.
“If we understand the process of acquisition better, then it could allow us to improve drug stewardship,” concludes Dr Quince.