How single-cell genomics can foil drug-resistant cancer
PhD student Silvia Ogbeide explains how she’s using the latest single-cell sequencing technologies to track drug resistance in cancer.
It’s likely you will have heard about antibiotic resistance in the news at some point, but did you know that cancer cells can become resistant to treatments over time, too? It’s a crucial battle to overcome if we’re to improve the outlook for patients receiving chemotherapy and other treatments.
Silvia Ogbeide is a PhD student in Iain Macaulay’s specialist single-cell genomics group, working on a Cancer Research UK-funded project to get to the bottom of drug resistance in cancer using the latest single-cell and organoid technologies.
Cancers usually start when a single cell goes rogue - multiplying in an uncontrolled way. Although the starting point is a single cell multiplying, that doesn’t mean all of the cells in a tumour are identical. There are a range of causes and drivers behind cancer growth, which makes selecting the most effective treatments a real challenge.
Cancer patients often undergo many cycles of chemotherapy to stop cancer from growing and spreading. Treatment is usually offered based on what has worked most effectively and was best tolerated in clinical trials. Unfortunately, these treatments are not always successful.
Cancer relapse in initial responders is dominated by cells that have either acquired resistant mutations after drug exposure or due to selection; that is, the treatment killed cells that were sensitive to the drug and left behind those inherently resistant, the frequency of which was low before the start of the treatment, but increased afterwards without any other competition.
The diversity of the cancer cells found in some tumours can dramatically limit the efficacy of targeted therapies and poses a significant challenge for precision medicine. Looking at evolutionary cues in cancer will help us understand the disease and provide insights that can help design novel therapeutic strategies that account for its adaptive nature, promote treatment responsiveness, and delay therapeutic resistance.
My PhD aims to exploit single-cell multi-omics techniques and bioinformatics tools to construct phylogenetic trees that reflect tumour evolution in the presence and absence of drug treatments. Essentially, we want to know how some cancer cells become resistant to a particular drug.
We want to trace how that happens to understand whether specific cells show resistance to treatments from the start or whether cells have acquired resistance over time. We want to know how long it takes to happen and reveal the pathways by which cells become resistant. To achieve this, I will perform parallel sequencing of single-cell genomes and transcriptomes (G&T-seq) on patient-derived organoids of colorectal cancer.
It depends on how many cycles that patients go through. In a perfect world we would like every patient to have a specific treatment.
That might involve looking into the genome, the transcriptome, or even the proteomics of the cancer, and seeing whether there is anything that could give you a little bit of resistance at the beginning and a lot of resistance at the end. What we’re working towards is personalised medicine, essentially, to develop technologies that can be applied clinically.
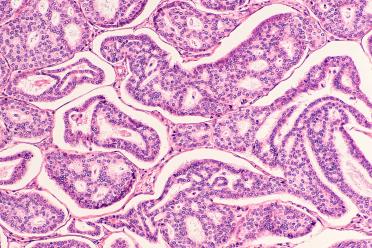
We’re working with collaborators in Milan and London, who are generating organoids from cancer biopsies. Organoids are essentially 3D models that allow us to look at a more realistic version of a cancer, rather than just a plate of cells - essentially they’re a small tumour. When you treat them with a drug, you get a much more similar response to how it would be in the body.
Those organoids are treated with different drugs in different concentrations using a microfluidics platform, which are then sent to me to do the single-cell sequencing - using G&T-seq to look at the genome and transcriptome of individual cells within them.
We’re also using a laser dissection method to get some spatial resolution, too. We can trace where the cell has come from in the organoid in relation to things such as stromal cells, fibroblasts and immune cells, and see whether that proximity has an effect on the transcriptome profile.


Single-cell sequencing gives you a much higher resolution than bulk sequencing. You could compare it to using a microscope, if you only have a 40x lens it won't give you as much resolution as if you look at 100x magnification.

I’ve heard it said that the best model is the patient, but of course you can’t get samples from the patient every time. That’s why it’s important to have all of the different information you can get - cell lines, mouse models, and these organoids. Having all of these gives you much more information about what the patient is going through.
Single-cell sequencing gives you a much higher resolution than bulk sequencing. You could compare it to using a microscope, if you only have a 40x lens it won't give you as much resolution as if you look at 100x magnification.
Take bulk sequencing, for example; if you have 100 cells, and only three of them have a specific mutation that confers drug resistance, there is a really low chance that you will pick them up - especially if they are not expressed.
With single-cell technologies, such as 10X Chromium, you can sequence 10,000 cells and, if you see something interesting within those cells, then you can go back and target them with antibodies and things like that. You can sort them, too, so that you have a higher chance of picking up cells of interest.

Contact our expert single-cell genomics team today to discuss a project.
Single-cell isolation platforms:
Single-cell sequencing protocols supported by our Genomics Services team:
During my undergraduate degree I did a placement year in a histopathology lab. I would receive samples of different cancers, such as mastectomies, or samples from the upper and lower gastrointestinal tract. I felt inspired to use these samples to try and find new ways to better treat the disease.
I wanted to continue studying cancer and did a Master’s in biomedical science, though I didn’t even think of doing a PhD after all that studying. Instead, I worked as a research technician for AstraZeneca, using histopathology and immunohistochemistry.
Eventually I realised that I wanted to learn more - to do something that would combine oncology with the molecular aspects I was interested in the most. When I saw this opportunity to work with Iain, it was a chance to get the best of both worlds.
I didn’t know much about single-cell at the time but reading some of the lab’s publications was fantastic and it looked like a great opportunity - most of all being able to work on something that could eventually be implemented in the clinic.

With single-cell technologies, such as 10X Chromium, you can sequence 10,000 cells and, if you see something interesting within those cells, then you can go back and target them with antibodies and things like that. You can sort them, too, so that you have a higher chance of picking up cells of interest.

It can be very easy to sequence your genome but, to pick up many mutations with the accuracy needed, you have to sequence very deep, which means that you have to spend more money on it. At the moment not everyone can do it.
Personalised medicine (also known as precision medicine) is a clinical strategy that aims to improve disease prognosis by tailoring health care to each patient’s molecular profile.
An example of personalised medicine would be offering chemotherapy in the form of receptor inhibitors in cases where the growth of breast cancer is fuelled by the excessive activation of the oestrogen and/or progesterone hormone receptors. In such cases, hormone therapy, usually combined with other medication, can drastically improve prognosis.
A different course of treatment may be offered to women without these sorts of genetic alterations, highlighting the importance of identifying breast cancer hormone status before any treatment is given. Hopefully, prescribing more effective drugs will also reduce the cost of health care.
Personalised treatment does not have to come into play after the onset of symptoms. It can also predict susceptibility to hereditary diseases given a known familiar history of germline mutations.
There are many advantages to personalised medicine but genomic research is not cheap, nor is it always translatable. Genomics data is already sharable but joining efforts between the research and clinical communities is essential for it to benefit more patients.