With an estimated 700,000 people dying every year due to drug-resistant infections, antibiotic resistance is one of the biggest threats to our global health and food security. More bacteria are becoming resilient to these widely-used drugs, resulting in the risk of a growing number of infections going untreated and leading to further strain on our medical care.
Antibiotics have been used by humans for decades, but the overuse and misuse of antibiotic drugs in humans and animals are having a negative effect. No longer a foolproof remedy, bacteria are becoming immune to current antibiotics; accelerated by the agricultural sector promoting growth and fighting disease, as well as global trade spreading resistant bugs.
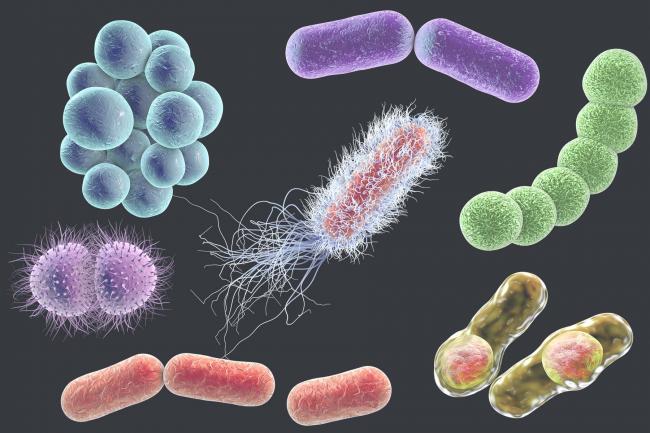
When antibiotics are used the targeted bacteria responds and adapts to survive, causing drug resistance and a shortage in antibiotic remedies for worldwide diseases such as TB, syphilis and diarrhoea.
Such antimicrobial resistance is accelerated by bacteria being exposed to antimicrobial drugs and can also lead to diseases such as salmonellosis, caused by salmonella which is difficult to treat. From the frequent use of antibiotics in livestock practices, the spread of foodborne disease is affecting 1 in 10 people and 33 million healthy life years are disappearing - with salmonella being one of the most pressing issues affecting our food chain.
We talk to Dr Matt Bawn at EI who is tackling Salmonella head-on by exploring a highly mutable, evolved strain to help answer why antibiotics are becoming less effective and improve our bodies’ antimicrobial armour.